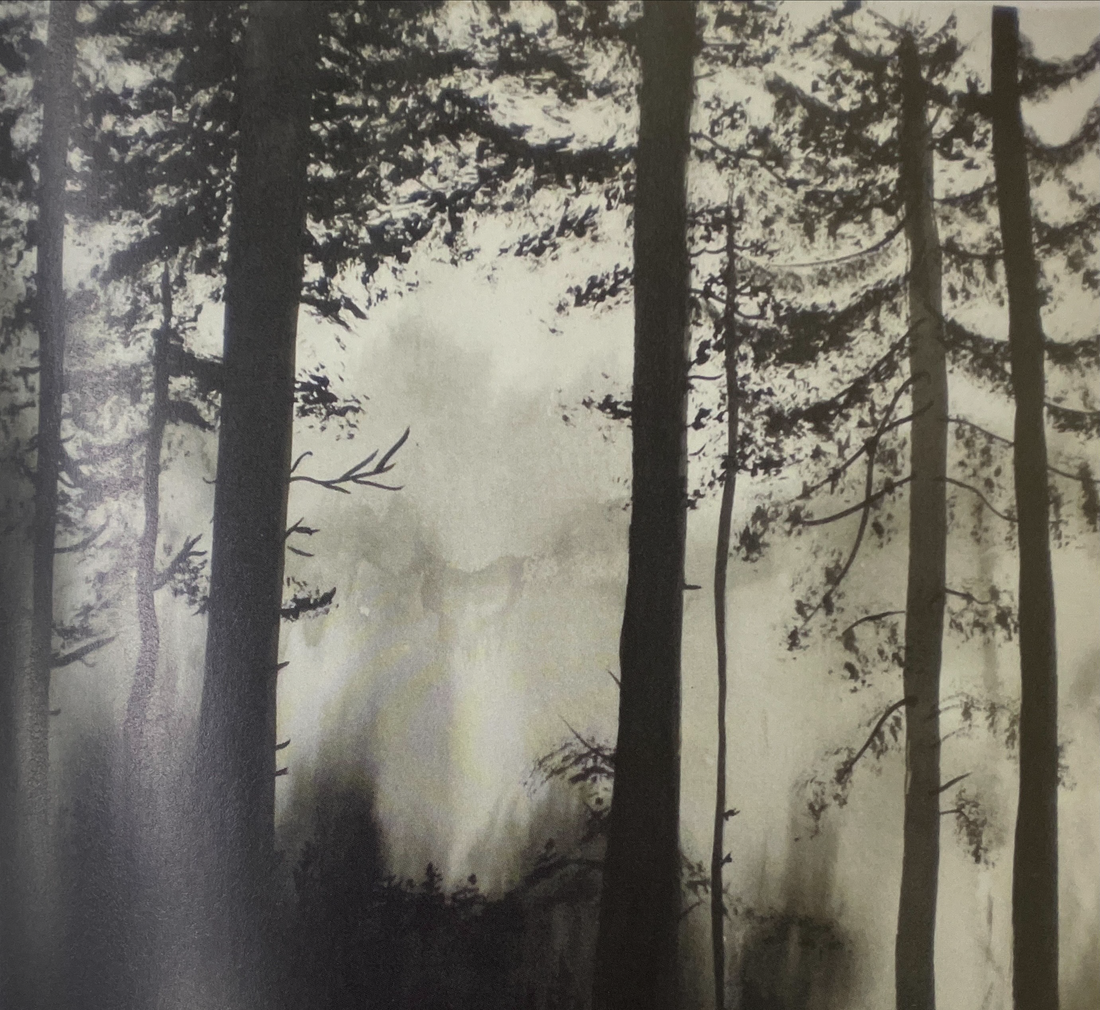
Featured Painting Title: The Forest
By Marianne McGlashan
"The picture is created using a monochromatic theme to illustrate the darkness of depression."
-
The 5 Steps First Aid Action Plan For Depression
ACTION I: Approach the person, assess and assist with any crisis
How to approach
If you think that someone you know may be depressed and in need of help, approach the person about your concerns. It is important to choose a suitable time when both you and the person are available to talk, as well as a space where you both feel comfortable. Let the person know that you are available to talk when they are ready; do not put pressure on the person to talk right away. It can be helpful to let the person choose the moment to open up. However, if the person does not initiate a conversation with you about how they are feeling, you should say something to them. You should respect the person's privacy and confidentiality unless you are concerned that the person is at risk of harming themselves or others.
As you talk with the person, be on the lookout for any indications that the person may be in crisis, you can ask them about how they are feeling and how long they have been feeling that way and move on to ACTION 2.
ACTION 2: Listen non-judgmentally
If you believe that the person is not in a crisis that needs immediate attention, you can engage the person in conversation, such as asking the person about how they are feeling and how long they have been feeling this way, Listening non-judgmentally is important at this stage as it can help the person to feel heard and understood, while not being judged in any way, this can make it easy for the person to feel comfortable to talk freely about their problems and to ask for help.
Tips for non-judgmental listening
It is very difficult to be entirely non-judgmental all of the time. We automatically make judgments about people from the minute we first see or meet them, based on their appearance, behaviour, and what they say. There is more to non-judgmental listening than simply trying not to make those judgments - it is about ensuring that you do not express your negative judgments, as this can get in the way of helping. If you have decided to approach someone with your concerns about them, it is a good idea to spend some time reflecting on your own state of mind first and ensure you are in the right frame of mind to express your concerns without being judgmental.
Although the focus of your conversation with the person you are helping is on their feelings, thoughts and experiences, you need to be aware of your own as well. Helping someone who is in distress may evoke an unexpected emotional response in you; you may find yourself feeling fearful, overwhelmed, sad or even irritated or frustrated.
In spite of any emotional response you have, you need to continue listening respectfully and avoid expressing a negative reaction to what the person says. This is sometimes difficult, and may be made more complex by your relationship with the person or your personal beliefs about their situation. You need to set aside these beliefs and reactions in order to focus on the needs of the person you are helping; their need to be heard, understood, and helped.
Remember that you are providing the person with a safe space to express themselves, and a negative reaction from you can prevent them from feeling that sense of safety.
Effective communication skills for non-judgmental listening
You can be an effective non-judgmental listener by paying special attention to two main areas:
• Your attitudes, and how they are conveyed. and
• Effective communication skills - both verbal and non-verbal
Attitudes
The key attitudes involved in non-judgmental listening are acceptance, genuineness and empathy.
Adopting an attitude of acceptance means respecting the person's feelings, persona values and experiences as valid, even if they are different from your own, or you disagree with them. You should not judge, criticise or trivialise what the person says because of your own beliefs or attitudes. Sometimes, this may mean withholding any and all judgments that you have made about the person and their circumstances, e.g. listen to the person without judging them as weak - these problems are not due to weakness or laziness - the person is trying to cope.
Genuineness means that what you say and do shows the person that they are accepted. This means not holding one set of attitudes while expressing another. Your body language and verbal cues should reinforce your acceptance of the person. For example, if you tell the person you accept and respect their feelings, but maintain a defensive posture or avoid eye contact, the person will know you are not being genuine.
Empathy means being able to imagine yourself in the other person's place, showing them that they are truly heard and understood by you.
This doesn't mean saying something glib such as "I understand exactly how you are feeling" - it is more appropriate to say that you can appreciate the difficulty that they may be going through. Remember that empathy is different from sympathy, which means feeling sorry for or pitying the person.
Verbal skills
Using the following simple verbal skills will show that you are listening:
• Ask questions which show that you genuinely care and want clarification about what they are saying.
• Check your understanding by re-stating what they have said and summarising facts and feelings.
• Listen not only to what the person says, but how they say it; their tone of voice and non-verbal cues will give extra clues about how they are feeling.
• Use minimal prompts, such as "I see" and "Ah" when necessary to keep the conversation going.
• Be patient, even when the person may not be communicating well, may be repetitive or may be speaking slower and less clearly than usual.
• Do not be critical or express your frustration at the person for having such symptoms.
• Avoid giving unhelpful advice such as "pull yourself together" or "cheer up". If this was possible the person would do it.
• Do not interrupt the person when they are speaking, especially to share your opinions or experiences.
• Avoid confrontation unless necessary to prevent harmful or dangerous acts.
Remember that pauses and silences are okay. Silence can be uncomfortable for many people, but the person may need time to think about what has been said, or may be struggling to find the words they need. Interrupting the silence may make it difficult for them to get back on track, and may damage the rapport you have been building. Consider whether the silence is awkward, or just awkward for you.
Non-verbal skills
Non-verbal communications and body language express a great deal. Good nonverbal skills show that you are listening, while poor non-verbal skills can damage the rapport between you and the person you are assisting and negate what you say.
Keep the following non-verbal cues in mind to reinforce your non-judgmental listening:
• Pay close attention to what the person says.
• Maintain comfortable eye contact. Don't avoid eye contact, but do avoid staring; you can do this by maintaining the level of eye contact that the person seems most comfortable with.
• Maintain an open body position. Don't cross your arms over your body, as this may appear defensive.
• If it is safe, sit down, even if the person is standing. This may seem less threatening.
• It is best to sit alongside the person and angled towards them, rather than directly opposite them.
• Do not fidget.
Cultural considerations for nonjudgmental listening
If you are assisting someone from a cultural background which is different from your own, you may need to adjust some of your verbal and non-verbal behaviours. For example, the person may be comfortable with a level of eye contact different from what you are used to, or may be used to more personal space.
If these differences are interfering with your ability to be an effective helper, it may be helpful to explore and try to understand the person's experiences, values or belief systems.
Be prepared to discuss what is culturally appropriate and realistic for the person, or seek advice from someone from their cultural background before speaking to them.
ACTION 3: Give support and information
Treat the person with respect and dignity
Each person's situation and needs are unique. It is important to respect the person's autonomy while considering the extent to which they are able to make decisions for themselves. Equally, you should respect the person's privacy and confidentiality unless you are concerned that the person is at risk of harming themselves or others.
Do not blame the person for their illness
Depression is a real health problem and the person cannot help being affected by depression. It is important to remind the person that they have a health problem and that they are not to blame for feeling "down."
Have realistic expectations for the person
You should accept the person as chey are and have realistic expectations for them. Everyday activities like cleaning the house, paying bills, or feeding the dog may seem overwhelming to the person. You should let them know that they are not weak or a failure because they have depression, and chat you don't chink less of them as a person. You should acknowledge that the person is not "faking", "lazy", "Weak" or "selfish."
Offer consistent emotional support and understanding
It is more important for you to be genuinely caring than for you to say all the "right things The person genuinely needs additional care and understanding to help them through their illness so you should be empathetic, compassionate and patient. People with depression are often overwhelmed by irrational fears; you need to be gently understanding of someone in this state. It is important to be patient, persistent and encouraging when supporting someone with depression. You should also offer the person kindness and attention, even if it is not reciprocated. Let the person know that they will not be abandoned. You should be consistent and predictable in your interactions with the person.
Give the person hope for recovery
You need to encourage the person to maintain hope by saying that, with time and treatment, they will feel better. Offer emotional support and hope of a more positive future in whatever form the person will accept.
Provide practical help
Ask the person if they would like any practical assistance with tasks, but be careful not to take over or encourage dependency.
Offer information
Ask the person if they would like some information about depression. If they do want some information, it is important that you give them resources that are accurate and appropriate to their situation. Don't assume that the person knows nothing about depression as they, or someone else close to them, may have experienced depression before.
What isn't supportive
• There's no point in just telling someone with depression to get better as they cannot "snap out of it" or "get over it."
• Do not be hostile or sarcastic when their responses are not what you usually expect of them. Rather, accept these responses of them.
as the best the person has to offer at that time.
• Do not adopt an over-involved or overprotective attitude towards someone who is depressed.
• Do not nag the person to try to get them to do what they normally would.
• Do not trivialise the person's experiences by pressuring them to "put a smile on their face," to "get their act together," or to "lighten up'
• Do not belittle or dismiss the person's feelings by attempting to say something positive like, "You don't seem that bad to me."
• Avoid speaking with a patronising tone of voice and do not use overly-compassionate looks of concern.
• Resist the urge to try to cure the person's depression or to come up with answers to their problems.
ACTION 4: Encourage the person to get appropriate professional help
Everybody feels down or sad at times, but it is important to be able to recognise when depression has become more than a temporary experience for someone and when to encourage that person to seek professional help. Professional help is warranted when depression lasts for weeks and affects a person's functioning in daily life. Many people with depressive disorders do not seek professional help. In Australia, only 59% of the people who had a depressive disorder in the past year received professional help for their problem.' Even when people do eventually seek help, they can wait for many years before doing so. These delays can affect their long-term recovery.
People with depressive disorders are more likely to seek help if someone close to them suggests it. Also, people can help a GP make a quicker diagnosis by telling the doctor directly about their psychological symptoms and that they may be suffering from depression.
Discuss options for seeking professional help
You should ask the person if they need help to manage how they are feeling. If they feel they do need help, discuss the options that they have for seeking help and encourage them to use these options. If the person does not know where to get help, offer to help them seek assistance. It is important to encourage the person to get appropriate professional help and effective treatment as early as possible. If the person would like you to support them by accompanying them to an appointment with a health professional, you must not take over completely; a person with depression needs to make their own decisions as much as possible. Depression is not always recognised by health professionals; it may take some time to get a diagnosis and find a healthcare provider with whom the person is able to establish a good relationship. You should encourage the person not to give up seeking appropriate professional help.
What if the person doesn't want help?
The person may not want to seek professional help. You should find out if there are specific reasons why this is the case. For example, the person might be concerned about finances, or about not having a doctor they like, or they might be worried they will be sent to hospital.
These reasons may be based on mistaken beliefs and you may be able to help the person overcome their worry about seeking help. If the person still doesn't want help after you have explored their reasons with them, let them know that if they change their mind in the future about seeking help they can contact you.
You must respect the person's right not to seek help unless you believe that they are at risk of harming themselves or others.
ACTION 5: Encourage other supports
Other people who can help
Encourage the person to consider other supports available to them, such as family, friends and support groups. Some people who experience depression find it helpful to meet with other people who have had similar experiences.
There is some evidence that these mutual help groups can help with recovery from depression and anxiety. Family and friends can also be an important source of support for a person who is depressed. Recovery from symptoms is quicker for people who feel supported by those around them.
People with mental illnesses who are hospitalised are less likely to receive flowers, get-well cards and other gifts which can lead them to have feelings of rejection. It is important chat family and friends provide the same sort of support to an ill person with a mental illness as they would to a person with a physical disorder. Providing the same support they would for a person who is physically ill can include sending get-well cards, flowers, phoning or visiting the person, and helping out if they cannot manage.
Self-help strategies
Self-help strategies are frequently used by people with depression. The person's ability and desire to use self-help strategies will depend on their interests and the severity of their depression. Therefore you should not be too forceful when trying to encourage the person to use self-help strategies.
Self-help strategies may be useful in conjunction with other treatments and may be suitable for people with less severe depression. It is important that severe or long lasting depression be assessed by a health professional. Not all self-help strategies are suitable for all people, because of side-effects or interactions with other medical illnesses or treatments. It is a good idea to discuss the appropriateness of self-help strategies with an appropriate professional.